Those of us with traumatic brain injuries (TBI) know how important sleep is for recovery from the injury. Sleeping plays a big part in helping our brains heal after a traumatic brain event. The more quality sleep, the better and faster the brain can heal.
Continuous learning about sleep facts, sleep disorders, and sleep hygiene is critical to our health. The following article breaks down the basics.
Sleeping well is in everybody’s self-interest—much of this is important information for everybody, whether there is a brain injury or not. There’s something here for everybody.
Let’s get started.
First, we all have something called a circadian rhythm, or our internal clock. The rhythm of our internal behaviors cycles through about 24 hours then starts all over again. The rhythms seem to be tied to day and night—we’re pretty much awake during the day and sleep at night.
According to the National Center for Biotechnology, sleep disorders affect 46% of TBI survivors. Some sleep disorders they cataloged were insomnia, bruxism (grinding teeth), sleep apnea, hypersomnia and narcolepsy (hypersomnia is the inability to stay awake during the day or prolonged nighttime sleep and narcolepsy is suddenly needing to fall asleep while engaged in an activity).
All these disorders and others can have significant effects on getting the kind of sleep needed for the brain to heal and may affect cognition.
Eight hours of sleep every night is the standard recommendation, but some people can do with less sleep and others need longer sleep periods.
But how does a brain injury survivor heal with a sleeping disorder that makes it difficult or impossible to get into a cycle of regular, uninterrupted and restful sleep?
How much and whether sleep is affected, like most other things with brain injury survivors, depends on which area of the brain is injured. Any brain injury that affects the hypothalamus, also called the sleep center, can result in sleep disorders. The number of brain injuries a person experiences can affect the quality and quantity of sleep. Untreated sleep disturbances following TBI can lead to serious consequences with respect to an individual’s cognitive functioning while awake.
There’s more.
While the brain is most active during the time we’re awake, it’s also active while we sleep.
In the normal course of doing its job, the brain accumulates toxins. One thing the brain does during sleep is to cleanse itself of those toxins and reinvigorate itself—and you in the process.
Dreaming is important too. One study showed that subjects who were awakened while they were dreaming showed the following:
- More tension and anxiety
- Depression
- Increased difficulty concentrating
- Lack of coordination
- Increased tendency to hallucinate
- Weight gain
It’s been thought for a long time that dreams can help solve problems*, incorporate and organize memories, process emotions and more.
(Note: *I think this is probably where the term sleep on it comes from).
Scientists studying sleep recommend what they call sleep hygiene for getting restful sleep and settling into a routine sleep pattern.
The CDC (Centers for Disease Control made these recommendations for sleep hygiene:
- Get up and go to bed at the same times every day, even on weekends
- Keep your bedroom dark, quiet, and at a comfortable temperature
- Keep electronics turned off
- Don’t eat large meals or drink caffeine close to bedtime
- Get plenty of exercise
If these don’t work, your doctor might recommend medication, either prescription or over the counter, to help with your sleeping challenges. Some sleep medications might cause other problems, though.
In the days right after the stroke that caused my brain injury, I had lots of trouble sleeping. I forced myself to stay awake because I was deathly afraid to sleep. I feared not waking up again or waking up in the hospital, which I did once and take my word for it, it was one of the least fun things I’ve ever done.
I might have benefited from a treatment called cognitive behavioral therapy (CBT). CBT is a technique that helps alter a patient’s negative associations with sleep. Examples of CBT are relaxation training and CBT1 for insomnia.
What your doctor recommends depends, obviously, on the cause of the sleep disorder.
Two examples:
For bruxism (again for grinding teeth in your sleep) it might be as simple as wearing a mouth guard at night.
Sleep apnea can have several causes and there are differing treatments accordingly. Continuing Positive Airway Pressure devices (CPAP machines) may be called for. Overweight persons can benefit from losing weight. A certain type of apnea may be treated by avoiding alcohol and certain sleep medications. Nasal sprays or breathing strips may help relieve other types of sleep apnea. But don’t take it from me; ask your doctor or visit a sleep center, if you have one near where you live.
That’s all for now. This is obviously just a broad overview of a subject with lots of moving parts. I’m not trying for a master’s degree here. But this should be enough information to get the ball rolling.
The bottom line is we spend on third of our lifetimes sleeping. Brain injury or not, we may as well do everything we can to make the most of that time.
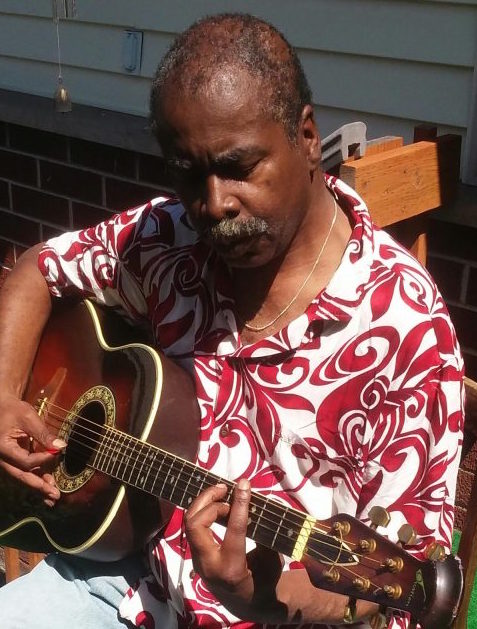 | Isaac Peterson grew up on an Air Force base near Cheyenne, Wyoming. After graduating from the University of Wyoming, he embarked on a career as an award-winning investigative journalist and as a semi-professional musician in the Twin Cities, the place he called home on and off for 35 years. He doesn’t mind it at all if someone offers to pick up his restaurant tab and, also, welcomes reader comments. Email him at isaac3rd@gmail.com. Read more articles by Isaac here; https://www.brainenergysupportteam.org/archives/tag/isaac-peterson |
|---|